POSIES Pathway
This pathway has been produced to aid clinicians caring for patients with malignant wounds. It aims to give guidance and support for a comprehensive, holistic assessment.
A clinical support pathway for Malignant wounds developed by clinicians; Sharon Gardner and Kathryn Taylor. POSIES is an acronym for:
Pain
Treatment plan:
Physical pain is a significant and complex phenomenon in malignant wounds. Pain can depend upon the area that the wound is located, the depth of the wound and its tissue invasion and damage and whether the nerves have been affected. Pain can also be due to macerated skin and inflammation as well as at dressing changes. It is important to consider the type and duration of pain.
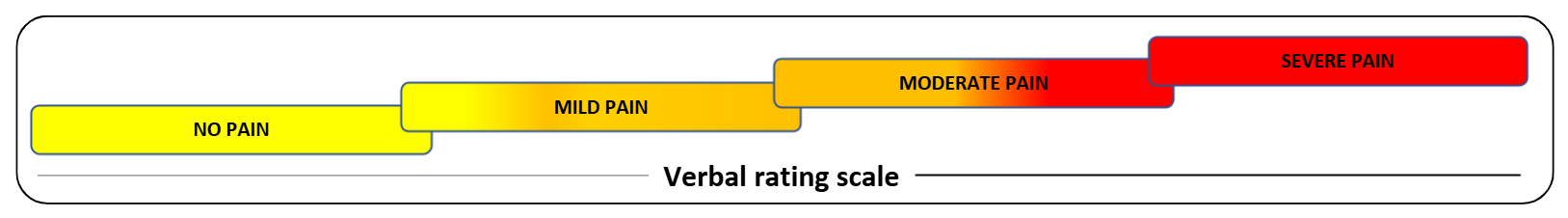
Severity: Ask the patient which word best describes their current level of pain (use a recognised pain assessment scale)
Odour
This occurs when the tissue on the wound has been deprived of oxygen and nutrients and becomes necrotic with bacterial growth on the tissue. Malodourous wounds can have a negative impact on patients quality of life.
Establish cause of odour and reverse if possible: Infection? If suspected cause of odour is infection, then please refer to section on Infection Slough/necrotic tissue in wound? If suspected cause of odour is slough/necrotic tissue in the wound then follow the below steps:
Treatment plan:
Aid autolytic debridement with one of the following products: (if appropriate and safe)
(Surgical, sharp and mechanical debridement is not recommended for fungating malignant wounds).
(Surgical, sharp and mechanical debridement is not recommended for fungating malignant wounds).
Odour controlling dressings should be considered as an adjunct to the above products if necessary (An activated charcoal dressings should be used for the containment of malodour and can be used as a secondary dressing over a non-adherent primary later).
European Oncology Nursing Society (2015) Recommendations for the care of patients with Malignant Fungating Wounds.
For further help or advice, please refer to Tissue Viability or specialist team.
Skin and Tissue
The skin surrounding the wound is very vulnerable to becoming sore and macerated due to exudate and frequent dressing changes, especially if there is an adhesive dressing being used.
The skin can also be very itchy (pruritis) which may be related to tumour growth.
If there is devitalised tissue in the wound, then please refer to the Odour section for debridement options.
Assessment of peri-wound skin:
Maceration
Excoriation
Itch
Infection
These wounds are at high risk of developing infection due to the compromised blood supply to the tumour which results in necrotic tissue. This can act as a medium for anaerobic and aerobic bacterial infection.
Bacterial infection can be expected and should be treated accordingly:
If you are concerned that the wound is clinically infected as evidenced by erythema, induration, increased pain, exudate, and fever, a wound swab and antibiotics should be considered. N.B. Only consider systemic antibiotics if the patient is unwell and pending a swab result.
Metronidazole Topical Gel is a commonly accepted treatment for both aerobic and anaerobic bacteria and is delivered topically, thus avoiding the side effects of oral Metronidazole. The British National Formulary advises that this should be prescribed for short term use usually daily for 5-7 days. The use of gel can cause increased exudate which may exacerbate problems if exudate is a challenge which should be considered and discussed with the patient prior to commencement.
Exudate and Bleeding
Malignant wounds depending on their characteristics could have a tendency to produce moderate to high levels of exudate. Exudate is due to tissue damage and increased leakage from blood vessels and can vary in amount.
Bleeding can be due to abnormal microcirculation, erosion, or compression of blood vessels by the tumour, decreased platelet function. It can also be caused by dressings adhering to wounds. Bleeding can be traumatic for both patients and their families/care givers. Prevention where possible is best, dressing changes and cleansing should only be performed where necessary.
Dressings should be removed carefully, using normal saline where required to minimize trauma (NICE, 2015). A medical adhesive removal product can also be used to minimize bleeding caused by removing adhesive dressings.
Radiotherapy and electrochemotherapy may be useful to control repetitive bleeds. Although fatal haemorrhage is rare, head and neck wounds that are adjacent to carotid arteries or those near the femoral artery are most likely to haemorrhage. The patient and family should be aware of this possibility and have sedative medications to hand should this event occur.
Bleeding Severity
Light Bleeding
Heavy Bleeding
Apply pressure to the wound and seek urgent medical advice (this is an emergency situation, and you should call 999, unless there is appropriate documentation to advice patient not for hospital admission).
Admission to hospital may be necessary depending on the stage of illness and the patients’ wishes. Patient wishes should be clearly documented in the plan of care.
For heavy and severe bleeding. Ensure the following medications are in the patient’s home:
Severe End of Life Bleeding
Anti- fibrinolytic – tranexamic acid may be useful but only prescribed after specialist advice. Tranexamic acid topically at dressing changes 500mg / 5mls, 5-10 mls –as a preventative measure – off licence drug. Oral antifibrinolytics three times a day are prescribed if there is a tendency to bleed or bled before.
Self
Malignant wounds can develop an array of emotions and psycho-social needs.
Depression, anxiety, low self-esteem, and loss of sexual intimacy are among some of the needs expressed by individuals. It is important for the patient to feel supported.
Continually assess the psychological and social needs of the patient during each visit/appointment by thorough holistic assessment.
Research has shown that families are often the ones to support the patients, and they themselves may experience extreme psychological distress. As part of assessment for ‘self’ families and care giver needs should be considered too.
Discuss with the patient options for referral to counselling support services, Macmillan nurses and other services for social support for themselves and family members.
Our Mission
We deliver the right and the most efficient outcomes to European Healthcare by providing products, services, and solutions.